Central Serous Chorioretinopathy or Central Serous Retinopathy (CSC or CSR) is a disorder that causes the accumulation of fluid under the macula in an otherwise healthy eye. This accumulation of fluid under the macula causes blurring of the central vision in the affected eye.
It is unclear what causes Central Serous Chorioretinopathy. However, we do know that CSC can be exacerbated by corticosteroid use. It is important to note that corticosteroids do not cause CSC, but if you have CSC, corticosteroids can make the condition worse. Corticosteroids that areare commonly associated with a worsening of CSC are:
Other hormone changes in the body can also make CSC worse such as pregnancy. Usually CSC may worsen in the third trimester of pregnancy and often resolves on its own after delivery.
The most common symptom of Central Serous Chorioretinopathy is blurriness, a smudge or gray spot near the center of your vision. A patient will usually notice this only in one eye, but closer examination will often find the presence of CSC in the other eye as well. When the fluid under the retina is not under the macula there are often no symptoms or apparent blurriness. (Note: the macula is the center of the retina and therefore is responsible for the center of our vision).
For reasons which are not known, Central Serous Chorioretinopathy affects men more commonly than women. CSC also affects middle-aged people more often than older adults, with most cases occurring between the ages of 30 and 50, although it can occur in someone in their 20s or 60s.
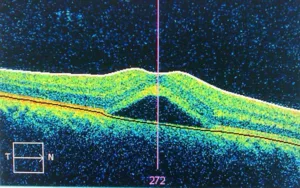 If you visit NYC Retina after noticing blurred vision in one or both eyes, we will begin with a vision test, followed by a complete eyeexam of both eyes by a retinal specialist looking for the fluid buildup under the retina/macula. A retinal scan using Optical Coherence Tomography (OCT) will be necessary to allow your physician to examine the affected area on a microscopic level. Another test that can help with identifying location of any fluid leakage is fluorescein angiography (IVFA). With IVFA, a safe, vegetable dye is injected into a vein in your arm. The dye travels through your vein to the blood vessels in the retina. Photos are then taken of your retina with a special camera. The camera can detect if the dye is leaking out of the blood vessels and pooling under the retina. Tthis will show up in the photos. Your retina specialist will review the OCT and IVFA with you and discuss your prognosis and treatment plan.
If you visit NYC Retina after noticing blurred vision in one or both eyes, we will begin with a vision test, followed by a complete eyeexam of both eyes by a retinal specialist looking for the fluid buildup under the retina/macula. A retinal scan using Optical Coherence Tomography (OCT) will be necessary to allow your physician to examine the affected area on a microscopic level. Another test that can help with identifying location of any fluid leakage is fluorescein angiography (IVFA). With IVFA, a safe, vegetable dye is injected into a vein in your arm. The dye travels through your vein to the blood vessels in the retina. Photos are then taken of your retina with a special camera. The camera can detect if the dye is leaking out of the blood vessels and pooling under the retina. Tthis will show up in the photos. Your retina specialist will review the OCT and IVFA with you and discuss your prognosis and treatment plan.
Prior to discussing any treatment options, please alert your retina specialist of any corticosteroids or hormone therapy that you may be taking. As mentioned above, commonly used corticosteroids in patients with CSC are: inhaler for asthma, nasal spray, skin cream prescribed by a dermatologist or injection of steroids in your joints/back.
The first step is discontinuing any corticosteroid use if it is safe for you to stop taking them. Discontinuing corticosteroid use should only be done after consulting with the doctor who prescribed them to ensure that it is safe to stop usage.
Of note, it is best to abstain from using even a small amount of low dose steroids as even that can cause an exacerbation of CSC. If steroids cannot be avoided, then CSC will be managed with observation and/or laser as mentioned.
The second step is to allow time for the subretinal fluid to clear on its own. Fortunately, the subretinal fluid often clears on its own with time and with no intervention.
If the fluid does not clear in 3-6 months, then micropulse laser is considered. Micropulse laser can be repeated multiple times if there is no resolution of subretinal fluid or improvement of your symptoms. If after multiple treatments with micropulse laser there is still persistent subretinal fluid, focal laser may be considered. If there is still no improvement then photodynamic therapy (PDT laser) and/or intravitreal injections may be considered as a last resort.
Once the fluid clears, the vision typically improves. The vision may improve partially or improve all the way back to normal. If the vision does not improve all the way back to normal it is usually due to damage done to the macula caused by the subretinal fluid. Unfortunately, this imperfect vision may be permanent.
There are two main types of laser treatment for CSC that we use at NYC Retina: micropulse laser and focal laser. Both types of laser are safe and effective. There are a few key differences that we will discuss below.
Micropulse laser is a shorter pulse of laser compared to conventional, continuous wave laser (focal).
The purpose of the laser is to stimulate the pigmented cells under the retina to reduce fluid leakage from the small blood vessels in the macula and facilitate the body’s removal of the excess fluid. If the fluid under the macula clears, the vision should improve.
Focal laser is a continuous pulse of laser as opposed to a “micro” pulse. This type of laser can be very effective in CSC when there is a clear, single leaking point or “hot spot” seen on the fluorescein angiogram. When focal laser treatment is successful, the fluid under the macula may clear leading to vision improvement. Of note, although the vision may improve, it may not improve all the way back to normal if permanent damage has been done to the macula and pigmented cells under the macula caused by the subretinal fluid.
Both of these laser treatments have a risk of not effectively clearing the fluid under the macula and failing to improve vision. There is also some risk of the laser leaving behind a small dark or blind spot near the center of the patient’s field of vision. The risk of a noticeable blind spot is low in both forms of laser, but the risk is lower with micropulse laser than with focal laser. Therefore, micropulse laser is often done first. Focal laser is done if micropulse laser does not work, or if there is a hot spot that would be conducive specifically to focal laser treatment. Both lasers are usually well tolerated and may be considered when the benefits outweigh the risks. Your retina specialist will discuss the risk/benefits with you at length prior to proceeding with any treatment option.
Besides avoiding usage of corticosteroids, there are some indications that a healthy lifestyle may decrease your risk of Central Serous Chorioretinopathy. These include getting enough sleep, minimizing alcohol and caffeine, and stress reduction through exercise and/or meditation.
Even successful treatment for Central Serous Chorioretinopathy does not guarantee that fluid buildup will not recur in the future in either eye. These recurrent episodes may be separated by months or years.
If nothing is done to alleviate fluid buildup and the fluid does not clear on its own, it may cause damage to the macula which may result in permanent worsening of vision.
If you notice any sudden changes in your vision, do not hesitate to schedule an appointment to discover the root of the issue. If untreated, many eye conditions can cause deterioration and permanent damage to your vision. Many cases of Central Serous Chorioretinopathy resolve on their own over time, but once the condition has been diagnosed, our retina specialists can work with you to find the best possible treatment option.